Summary :
More than 1.2 million people – and potentially millions more – died in 2019 as a direct result of antibiotic-resistant bacterial infections, according to the most comprehensive estimate to date of the global impact of antimicrobial resistance (AMR).
The analysis of 204 countries and territories, published in The Lancet, reveals that AMR is now a leading cause of death worldwide, higher than HIV/AIDS or malaria. It shows that many hundreds of thousands of deaths now occur due to common, previously treatable infections – such as lower respiratory and bloodstream infections – because the bacteria that cause them have become resistant to treatment.
The report highlights an urgent need to scale up action to combat AMR, and outlines immediate actions for policymakers that will help save lives and protect health systems. These include optimising the use of existing antibiotics, taking greater action to monitor and control infections, and providing more funding to develop new antibiotics and treatments.
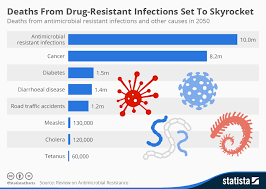
Study co-author Professor Chris Murray, of the Institute for Health Metrics and Evaluation at the University of Washington, USA, said: “These new data reveal the true scale of antimicrobial resistance worldwide, and are a clear signal that we must act now to combat the threat. Previous estimates had predicted 10 million annual deaths from antimicrobial resistance by 2050, but we now know for certain that we are already far closer to that figure than we thought. We need to leverage this data to course-correct action and drive innovation if we want to stay ahead in the race against antimicrobial resistance.” [1]
Estimates of the health impacts of AMR have been published for several countries and regions, and for a small number of pathogen-drug combinations in a wider range of locations. However, until now no estimates have covered all locations and a broad range of pathogens and drug combinations.
The new Global Research on Antimicrobial Resistance (GRAM) report estimates deaths linked to 23 pathogens and 88 pathogen-drug combinations in 204 countries and territories in 2019. Statistical modelling was used to produce estimates of the impact of AMR in all locations – including those with no data – using 471 million individual records obtained from systematic literature reviews, hospital systems, surveillance systems, and other data sources.
antibiotic-resistant bacterial infections
Disease burden was estimated in two ways: deaths caused directly by AMR (i.e. deaths that would not have occurred had the infections been drug-susceptible and therefore more treatable), and deaths associated with AMR (i.e. where a drug-resistant infection was implicated in deaths, but resistance itself may or may not have been the direct cause). Deaths caused by and associated with AMR were calculated for 204 countries and territories and reported for 21 global regions and seven super-regions.
The analysis shows AMR was directly responsible for an estimated 1.27 million deaths worldwide, and associated with an estimated 4.95 million deaths, in 2019. HIV/AIDS and malaria have been estimated to have caused 860,000 and 640,000 deaths, respectively, in 2019.[2]
Drug-resistance in lower respiratory infections – such as pneumonia – had the greatest impact on AMR disease burden, causing more than 400,000 deaths and associated with more than 1.5 million deaths. Drug resistance in bloodstream infections – which can lead to the life-threatening condition sepsis – caused around 370,000 deaths and was associated with nearly 1.5 million deaths. Drug resistance in intra-abdominal infections – commonly caused by appendicitis – led directly to around 210,000 deaths and was associated with around 800,000.
While AMR poses a threat to people of all ages, young children were found to be at particularly high risk, with around one in five deaths attributable to AMR occurring in children aged under five years.
Deaths caused directly by AMR were estimated to be highest in Sub-Saharan Africa and South Asia, at 24 deaths per 100,000 population and 22 deaths per 100,000 population, respectively. AMR was associated with 99 deaths per 100,000 in Sub-Saharan Africa and 77 deaths per 100,000 in South Asia. In high-income countries, AMR led directly to 13 deaths per 100,000 and was associated with 56 deaths per 100,000. (For regional data, see Table 3 in the paper).
“In the past, we all thought that you had to be rich enough to use a lot of antibiotics inappropriately to have this problem,” he says. “But that’s not the case.”
The researchers calculate that deaths caused directly by antibiotic resistance are the highest in sub-Saharan Africa, causing 24 deaths per 100,000 population annually, compared with an average fatality rate of 13 per 100,000 in high-income countries. Australia has the lowest mortality rate globally from antibiotic resistance, at 6 deaths per 100,000.
“That resistance out there is actually now one of the leading causes of death in the world,” says Dr. Chris Murray, the director of the Institute for Health Metrics and Evaluation. Murray is one of the authors of a new study, published in the medical journal The Lancet, that finds that in 2019, drug-resistant infections directly killed 1.2 million people and played a role in 5 million more deaths worldwide. Murray and his colleagues set out to quantify how much of a problem antibiotic resistance is globally, and they found that bacteria are mutating to evade antibiotics at a pace far faster than many researchers had previously forecast.
These deadly new strains of bacteria are causing untreatable blood infections, fatal pneumonia, relentless urinary tract infections, gangrenous wounds and terminal cases of sepsis, among other conditions.
Of the 23 pathogens studied, drug resistance in six alone (E. coli, S. aureus, K. pneumoniae, S. pneumoniae, A. baumannii, and P. aeruginosa) led directly to 929,000 deaths and was associated with 3.57 million. One pathogen-drug combination – methicillin-resistant S. aureus, or MRSA – directly caused more than 100,000 deaths in 2019, while six more each caused between 50,000 and 100,000 deaths.
Across all pathogens, resistance to two classes of antibiotics often considered the first line defence against severe infections – fluoroquinolones and beta-lactam antibiotics – accounted for more than an estimated 70% of deaths caused by AMR.
The health impact of pathogens varied widely based on location, with deaths attributable to AMR in Sub-Saharan Africa most often caused by S. pneumonia (16% of deaths) or K. pneumonia (20%), while around half of deaths attributable to AMR in high-income countries were caused by S. aureus (26%) or E. coli (23%).
“With resistance varying so substantially by country and region, improving the collection of data worldwide is essential to help us better track levels of resistance and equip clinicians and policymakers with the information they need to address the most pressing challenges posed by antimicrobial resistance. We identified serious data gaps in many low-income countries, emphasising a particular need to increase laboratory capacity and data collection in these locations,” said study co-author Prof Christiane Dolecek, GRAM scientific lead based in Oxford University’s Centre for Tropical Medicine and Global Health and the Mahidol Oxford Tropical Medicine Research Unit (MORU).[1]
The authors acknowledge some limitations to their study. Limited availability of data for some parts of the world, particularly many LMICs, may limit the accuracy of estimates in these locations as this required strong methodological assumptions to be made in the analysis. Combining and standardising data from a wide variety of sources also led to some potential sources of bias, including misclassification of community- or hospital-acquired infections, and inconsistency in the distinction between drug resistant and susceptible infections. There is also the potential for selection bias in passive surveillance systems, and hospital microbial data from LMICs may skew towards more urban populations or more severe disease.
Writing in a linked Comment, Dr Ramanan Laxminarayan, Center for Disease Dynamics, Economics & Policy (USA), who was not involved in the study, said: “From being an unrecognised and hidden problem, a clearer picture of the burden of AMR is finally emerging. Even the lower end of 911,000 deaths estimated by Murray and colleagues is higher than the number of deaths from HIV, which attracts close to US$50 billion each year. However, global spending on addressing AMR is probably much lower than that. This needs to change. Spending needs to be directed to preventing infections in the first place, making sure existing antibiotics are used appropriately and judiciously, and to bringing new antibiotics to market. Health and political leaders at local, national, and international levels need to take seriously the importance of addressing AMR and the challenge of poor access to affordable, effective antibiotics.”
Antimicrobial Resistance Collaborators.
Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis.
The Lancet, 2022. doi: 10.1016/S0140-6736(21)02724-0
Antibiotic-Resistant Bacterial Infections
The germs are listed in three categories—urgent, serious, and concerning—based on level of concern to human health. The report also includes a Watch List with three threats that have not spread widely in the U.S. but could become common without continued aggressive action.
The 2019 AR Threats Report is intended to:
- Serve as a reference for information on antibiotic resistance
- Provide the latest U.S. antibiotic resistance burden estimates for human health
- Highlight emerging areas of concern and additional action needed
What are antimicrobials?
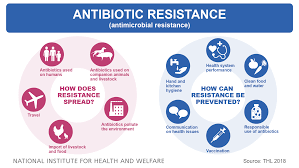
Antimicrobials – including antibiotics, antivirals, antifungals and antiparasitics – are medicines used to prevent and treat infections in humans, animals and plants.
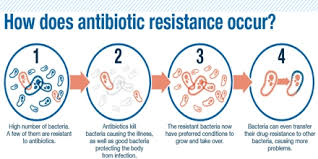
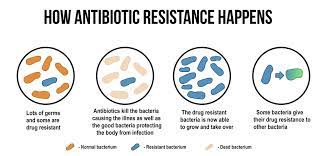
What is antimicrobial resistance?
Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat.
Why is antimicrobial resistance a global concern?
The emergence and spread of drug-resistant pathogens that have acquired new resistance mechanisms, leading to antimicrobial resistance, continues to threaten our ability to treat common infections. Especially alarming is the rapid global spread of multi- and pan-resistant bacteria (also known as “superbugs”) that cause infections that are not treatable with existing antimicrobial medicines such as antibiotics.
The clinical pipeline of new antimicrobials is dry. In 2019 WHO identified 32 antibiotics in clinical development that address the WHO list of priority pathogens, of which only six were classified as innovative. Furthermore, a lack of access to quality antimicrobials remains a major issue. Antibiotic shortages are affecting countries of all levels of development and especially in health- care systems.
Antibiotics are becoming increasingly ineffective as drug-resistance spreads globally leading to more difficult to treat infections and death. New antibacterials are urgently needed – for example, to treat carbapenem-resistant gram-negative bacterial infections as identified in the WHO priority pathogen list. However, if people do not change the way antibiotics are used now, these new antibiotics will suffer the same fate as the current ones and become ineffective.
The cost of AMR to national economies and their health systems is significant as it affects productivity of patients or their caretakers through prolonged hospital stays and the need for more expensive and intensive care.
Without effective tools for the prevention and adequate treatment of drug-resistant infections and improved access to existing and new quality-assured antimicrobials, the number of people for whom treatment is failing or who die of infections will increase. Medical procedures, such as surgery, including caesarean sections or hip replacements, cancer chemotherapy, and organ transplantation, will become more risky.
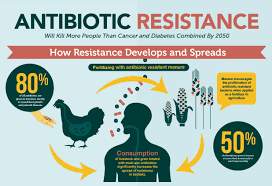
What accelerates the emergence and spread of antimicrobial resistance?
AMR occurs naturally over time, usually through genetic changes. Antimicrobial resistant organisms are found in people, animals, food, plants and the environment (in water, soil and air). They can spread from person to person or between people and animals, including from food of animal origin. The main drivers of antimicrobial resistance include the misuse and overuse of antimicrobials; lack of access to clean water, sanitation and hygiene (WASH) for both humans and animals; poor infection and disease prevention and control in health-care facilities and farms; poor access to quality, affordable medicines, vaccines and diagnostics; lack of awareness and knowledge; and lack of enforcement of legislation.
Present situation
Drug resistance in bacteria
For common bacterial infections, including urinary tract infections, sepsis, sexually transmitted infections, and some forms of diarrhoea, high rates of resistance against antibiotics frequently used to treat these infections have been observed world-wide, indicating that we are running out of effective antibiotics. For example, the rate of resistance to ciprofloxacin, an antibiotic commonly used to treat urinary tract infections, varied from 8.4% to 92.9% for Escherichia coliand from 4.1% to 79.4% for Klebsiella pneumoniae in countries reporting to the Global Antimicrobial Resistance and Use Surveillance System (GLASS).
Klebsiella pneumoniae are common intestinal bacteria that can cause life-threatening infections. Resistance in K. pneumoniae to last resort treatment (carbapenem antibiotics) has spread to all regions of the world. K. pneumoniae is a major cause of hospital-acquired infections such as pneumonia, bloodstream infections, and infections in newborns and intensive-care unit patients. In some countries, carbapenem antibiotics do not work in more than half of the patients treated for K. pneumoniae infections due to resistance.
Resistance to fluoroquinolone antibiotics in E. coli, used for the treatment of urinary tract infections, is widespread.
There are countries in many parts of the world where this treatment is now ineffective in more than half of patients.
Colistin is the only last resort treatment for life-threatening infections caused by carbapenem resistant Enterobacteriaceae (i.e. E.coli, Klebsiella, etc). Bacteria resistant to colistin have also been detected in several countries and regions, causing infections for which there is no effective antibiotic treatment at present.
The bacteria Staphylococcus aureus are part of our skin flora and arealso a common cause of infections both in the community and in health-care facilities. People with methicillin-resistant Staphylococcus aureus (MRSA) infections are 64% more likely to die than people with drug-sensitive infections.
In 2019, a new AMR indicator was included in the SDG monitoring framework. This indicator monitors the frequency of bloodstream infections due to two specific drug resistant pathogens: methicillin-resistant Staphylococcus aureus (MRSA); and E. coli resistant to third generation cephalosporins (3GC). In 2019, 25 countries, territories and areas provided data to GLASS on blood-stream infections due to MRSA and 49 countries provided data on bloodstream infections due to E.coli. While the data are still not nationally representative, the median rate observed for methicillin-resistant S. aureus was 12.11% (IQR 6.4–26.4) and that for E. coli resistant to third generation cephalosporins was 36.0% (IQR 15.2–63.0).
Widespread resistance in highly variable strains of N. gonorrhoeae has compromised the management and control of gonorrhoea. Resistance has rapidly emerged to sulphonamides, penicillins, tetracyclines, macrolides, fluoroquinolones, and early generation cephalosporins. Currently, in most countries, the injectable extended-spectrum cephalosporin (ESC) ceftriaxone is the only remaining empiric monotherapy for gonorrhoea.
Drug resistance in mycobacterium tuberculosis
Antibiotic resistant Mycobacterium tuberculosis strains are threatening progress in containing the global tuberculosis epidemic. WHO estimates that, in 2018, there were about half a million new cases of rifampicin-resistant TB (RR-TB) identified globally, of which the vast majority have multi-drug resistant TB (MDR-TB), a form of tuberculosis that is resistant to the two most powerful anti-TB drugs. Only one-third of the approximately half a million people who developed MDR/RR-TB in 2018 were detected and reported. MDR-TB requires treatment courses that are longer, less effective and far more expensive than those for non-resistant TB. Less than 60% of those treated for MDR/RR-TB are successfully cured.
In 2018, an estimated 3.4% of new TB cases and 18% of previously treated cases had MDR-TB/ RR-TB and the emergence of resistance to new ‘last resort’ TB drugs to treat drug resistant TB poses a major threat.
Drug resistance in viruses
Antiviral drug resistance is an increasing concern in immunocompromised patient populations, where ongoing viral replication and prolonged drug exposure lead to the selection of resistant strains. Resistance has developed to most antivirals including antiretroviral (ARV) drugs.
All antiretroviral (ARV) drugs, including newer classes, are at risk of becoming partly or fully inactive because of the emergence of drug-resistant HIV (HIVDR). People receiving antiretroviral therapy can acquire HIVDR, and people can also be infected with HIV that is already drug resistant. Levels of pretreatment HIVDR (PDR) to non-nucleoside reverse-transcriptase inhibitors (NNRTIs) among adults initiating first-line therapy exceeded 10% in the majority of the monitored countries in Africa, Asia and Latin America. The prevalence of PDR among infants is alarmingly high. In sub-Saharan Africa, over 50% of the infants newly diagnosed with HIV carry a virus that is resistant to NNRTI. Informed by these findings, latest WHO ARV guidelines now recommend the adoption of a new drug, dolutegravir, as the preferred first-line treatment for adults and children. The use of this drug is particularly urgent in averting the negative effects of resistance to NNRTIs.
Increasing levels of resistance have important economic implications since second- and third-line regimens are much more expensive than first-line drugs. WHO’s HIV drug resistance programme is monitoring the transmission and emergence of resistance to older and newer HIV drugs around the globe.
Drug resistance in malaria parasites
The emergence of drug-resistant parasites poses one of the greatest threats to malaria control and results in increased malaria morbidity and mortality. Artemisinin-based combination therapies (ACTs) are the recommended first-line treatment for uncomplicated P. falciparum malaria and are used by most malaria endemic countries. ACTs are a combination of an artemisinin component and a partner drug. In the WHO Western Pacific Region and in the WHO South-East Asia Region, partial resistance to artemisinin and resistance to a number of the ACT partner drugs has been confirmed in Cambodia, Lao People’s Democratic Republic, Myanmar, Thailand, and Viet Nam through studies conducted between 2001 and 2019. This makes selecting the right treatment more challenging and requires close monitoring.
In the WHO Eastern Mediterranean Region, P. falciparum resistance to sulfadoxine-pyrimethamine led to artesunate-sulfadoxine-pyrimethamine failures in some countries, necessitating a change to another ACT.
In Africa, evidence has recently been published showing emergence of mutations linked to partial artemisinin resistance in Rwanda. So far, ACTs that have been tested remain highly efficacious. However, further spread of resistance to artemisinin and ACT partner drugs could pose a major public health challenge and jeopardize important gains in malaria control.
Drug resistance in fungi
The prevalence of drug-resistant fungal infections is increasing and exasperating the already difficult treatment situation. Many fungal infections have existing treatability issues such as toxicity especially for patients with other underlying infections (e.g. HIV). Drug-resistant Candida auris, one of the most common invasive fungal infections, is already widespread with increasing resistance reported to fluconazole, amphotericin B and voriconazole as well as emerging caspofungin resistance.
This is leading to more difficult to treat fungal infections, treatment failures, longer hospital stays and much more expensive treatment options. WHO is undertaking a comprehensive review of fungal infections globally and will publish a list of fungal pathogens of public health importance, along with an analysis of the antifungal development pipeline.